kidney transplantation
Comprehensive Guide to Kidney Transplantation: Eligibility, Procedure, and Post-Transplant Care.
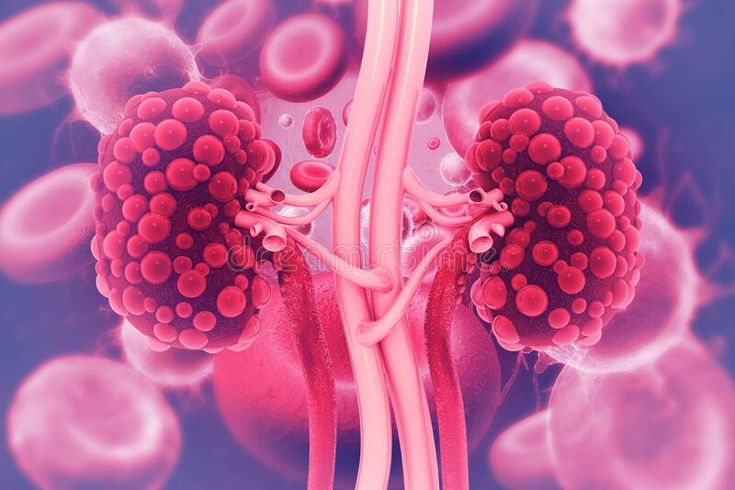
Kidney transplantation stands as a beacon of hope for individuals grappling with end-stage renal disease (ESRD). It represents a life-changing opportunity by substituting a failed kidney with a healthy one from a donor. This detailed guide aims to delve deeper into the intricate process of kidney transplantation, encompassing the nuances of eligibility criteria, the surgical intricacies, and the critical aspects of post-transplant care.
Eligibility Criteria for Kidney Transplantation: The road to kidney transplantation commences with stringent eligibility criteria. Patients who are
considered suitable candidates for this life-altering procedure typically fall within certain parameters:
Diagnosis of End-Stage Renal Disease: Candidates must exhibit a condition necessitating either dialysis or transplantation due to severe kidney dysfunction.
General Health Assessment: Being in good overall health without uncontrolled infections, cancers, or comorbidities that might jeopardize the success of the transplantation.
Compliance and Commitment: Demonstrating adherence to medical therapies and showcasing commitment to follow post-transplant care instructions diligently.
Evaluation Process for Transplant: The evaluation process is a meticulous and comprehensive assessment involving various medical tests, psychological evaluations, and consultations with a multidisciplinary transplant team. This team comprises nephrologists, transplant surgeons, social workers, dietitians, and other healthcare professionals. The tests encompass blood type matching, tissue compatibility, overall health assessments, and an evaluation of potential risks associated with the procedure.
Donor Selection and Compatibility: The quest for a suitable kidney involves sourcing from deceased or living donors. Living donors, often relatives or willing individuals, undergo thorough assessments to ensure compatibility. Compatibility tests involve blood type matching, tissue compatibility, and thorough evaluations to guarantee a viable match between the donor and recipient, thereby reducing the risk of rejection.
Surgical Procedure: Once a compatible donor is identified, the transplant surgery is scheduled. The surgical procedure involves placing the new kidney in the lower abdomen of the recipient. The duration of the surgery can span several hours, and patients typically remain hospitalized for about a week to facilitate recovery and close monitoring.
Post-Transplant Care and Management:
The success of a kidney transplant hinges on meticulous post-operative care and management:
Immunosuppressant Medications: Essential for preventing the body from rejecting the transplanted kidney. Adherence to the prescribed medication regimen is paramount. Ongoing Monitoring and Follow-ups: Regular check-ups to assess kidney function, medication levels, and overall health are imperative.
Embracing Lifestyle Modifications: Adopting a healthy lifestyle inclusive of a balanced diet, regular exercise, refraining from smoking, and moderating alcohol consumption significantly contribute to sustaining kidney health.
Psychosocial Support: Coping with the emotional and psychological aspects post-transplantation is critical. Support groups or counselling sessions can aid recipients in navigating the intricacies of life after transplantation.
Risks and Complications:
While kidney transplantation boasts high success rates, potential risks and complications persist
Risk of Rejection: The body’s immune system may perceive the transplanted kidney as foreign and mount an immune response. Immunosuppressant drugs play a pivotal role in preventing rejection.
Susceptibility to Infections: Immunosuppressants can heighten the risk of infections. Prudent hygiene practices and vigilant monitoring are imperative.
Side Effects of Medication: Immunosuppressants may trigger side effects such as elevated blood
pressure, diabetes, or weakened bones (osteoporosis).
Conclusion:
Kidney transplantation offers renewed hope and an improved quality of life for individuals battling ESRD. The journey involves a difficult examination, a complex surgical procedure, and a lifetime commitment to post-transplant care. Recipients can enjoy the benefits of improved health and well- being thanks to developments in medical technology and dedication to post-transplant protocols. It’s important to acknowledge that the path to kidney transplantation is unique for each individual. Seeking guidance and consultation from healthcare professionals and a dedicated transplant team is indispensable to comprehend personalized care plans and post transplantation expectations.
How vikgraf 1mg tablets helps you?
Vikgraf 1mg is a crucial medication for individuals who’ve undergone kidney transplantation. After the transplant, the body’s immune system can recognize the new kidney as foreign and attempt to reject it. Tacrolimus works by suppressing specific immune cells responsible for triggering this rejection response, helping to prevent the body from attacking the transplanted kidney. Usually, it’s part of a long-term treatment plan, used to maintain the kidney’s function by keeping the immune system in check. Doctors regularly monitor Tacrolimus levels through blood tests to ensure it remains within the right range for effectiveness while minimizing potential side effects. Often, it’s prescribed alongside other medications that complement its action, allowing for a lower overall doseand reducing the risk of adverse effects.